There is an increasing need for treatments that are effective in non-albicans species1-4,7
Over 90% of all invasive candidiasis (IC) cases are attributable collectively to just five species: C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, and C. krusei.1
However, since the 1980s and 1990s there has been a notable shift in the prevalence of these species. For example, the proportion of C. albicans has decreased from 70–80% to approximately 40–60% in Europe.2
In contrast, non-albicans species have been on the rise, now accounting for more than 50% of invasive candidiasis cases:2,3
- C. glabrata is increasing in Northern Europe, the US, and Australia2
- C. parapsilosis is becoming more prevalent in Southern Europe, China, and Latin America.2
Among the non-albicans species responsible for disease, C. glabrata stands out as the second-leading cause of nosocomial systemic Candida infections, with an associated 30-day mortality of 53.8%.4
Candida in Europe
Country species distribution for countries with ≥18 isolates from the ECMM Candida III study2
Referred isolates
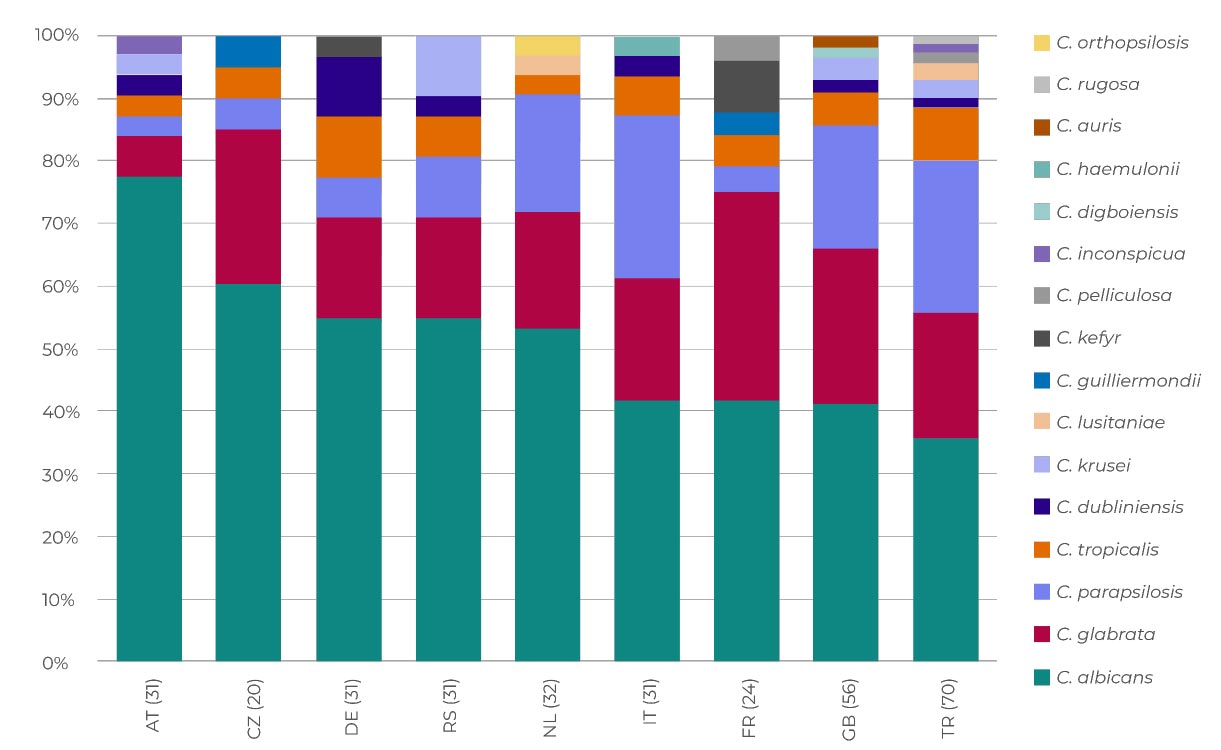
Adapted from Arendrup MC, et al. 2023.2
Countries are represented by their respective two-letter country code (listed in the abbreviations section below). The number of isolates is indicated in parenthesis. Countries are sorted according to descending proportion of C. albicans.
See how to overcome the challenges of managing non-albicans species
Increasing azole resistance
The widespread use of fluconazole has been linked to a rise in fluconazole-resistant strains, affecting both C. albicans and other Candida species.5,6
An analysis of 20,788 invasive Candida isolates, sourced from the global SENTRY programme between 1997 and 2016, highlighted an increase in resistance to fluconazole across multiple Candida strains.6
- In one study, (n=49) the overall rate of fluconazole resistance in C. glabrata was ~10%5
- Research from this study showed that 33% of patients with C.parapsilosis (n=194) were resistant to fluconazole5
Discover more about azole resistance
▼REZZAYO® (rezafungin) click for GB prescribing information or NI prescribing information
AT, Austria; CZ, Czech Republic; DE, Germany; ECCM, European Confederation of Medical Mycology; FR, France; GB, Great Britain; IC, invasive candidiasis; IT, Italy; NL, Netherlands; RS, Serbia; TR, Turkey.
- Antinori S, et al. Eur J Intern Med. 2016;34:21–28.
- Arendrup MC, et al. J Infect. 2023;S0163-4453(23)00451-6.
- McCarty TP, et al. Infect Dis Clin North Am. 2021;35(2):389–413.
- Gupta A, et al. Indian J Crit Care Med. 2015;19(3):151–154.
- Mesini A, et al. Mycoses. 2020;63(4):361–368.
- Pfaller MA, et al. Open Forum Infect Dis. 2019;6(Suppl 1):S79–S94.
- World Health Organization. WHO fungal priority pathogens list to guide research, development and public health action, 2022. [Accessed February 2024.] www.who.int/publications/i/item/9789240060241.
Adverse events should be reported. Reporting forms and information can be found at http://yellowcard.mhra.gov.uk/.
Adverse events should also be reported to Napp Pharmaceuticals Limited on 01223 424444 or drugsafetyUKandROI@mundipharma.com.









